Seeing blood in stools can be alarming, often prompting immediate concerns about serious conditions like colorectal cancer or inflammatory bowel disease. The logical next step is usually a colonoscopy, a thorough examination of the colon and rectum. But what happens when the colonoscopy comes back completely normal?
A normal colonoscopy can be both a relief and a source of confusion. If there’s no obvious source of rectal bleeding, what’s causing it, and what should be done next? Understanding the potential explanations and next steps can help patients navigate this uncertain territory with more clarity and confidence.
First, Understand What a Normal Colonoscopy Means
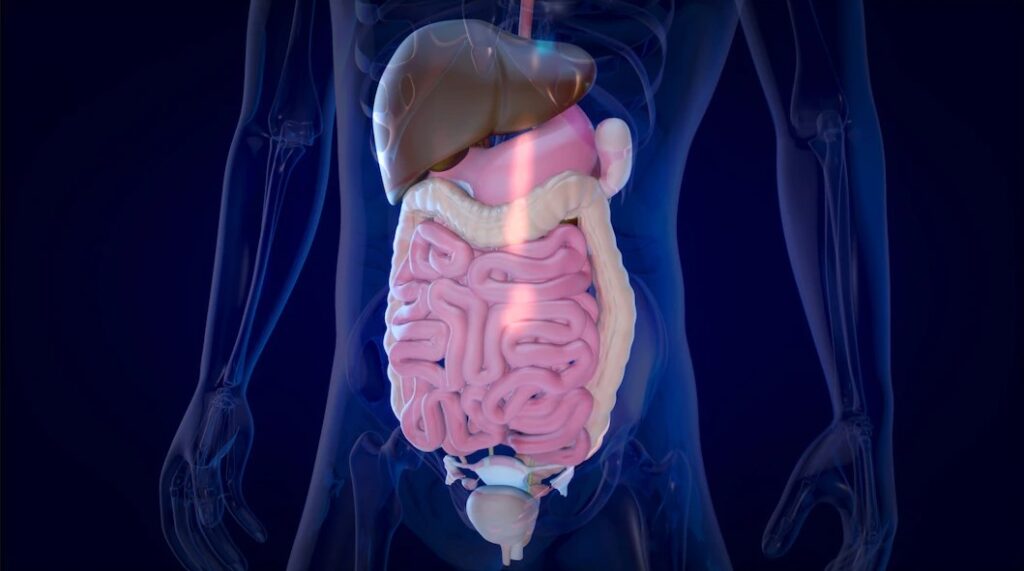
A normal colonoscopy means that no visible abnormalities were found in the colon or rectum. That includes no polyps, tumors, ulcers, inflammation, or diverticula significant enough to explain the bloody stool.
This result generally rules out many serious conditions, including colorectal cancer, ulcerative colitis, and large bleeding polyps. It’s an important piece of reassurance, but it doesn’t always mean the investigation is over. In some cases, the bleeding may originate from areas not examined during a colonoscopy or from smaller issues that aren’t easily visible.
Consider Other Sources of Bleeding
When a colonoscopy is normal but blood in stools persists, doctors begin to consider other possible sources of the bleeding. One common cause is anal fissures, which are small tears in the skin around the anus. These often result from passing hard stools and can cause bright red blood on the toilet paper or surface of the stool.
Hemorrhoids are another frequent culprit. These swollen veins in the rectum or anus can bleed, especially after straining during bowel movements. While internal hemorrhoids may be seen during a colonoscopy, small or external ones might be missed if not actively bleeding at the time of the exam.
In some cases, the bleeding may come from upper gastrointestinal sources, such as the stomach or small intestine. This can be the case if the blood appears dark or tar-like, a condition called melena. If an upper GI source is suspected, an upper endoscopy or capsule endoscopy may be the next step.
Don’t Overlook Medications and Lifestyle Factors
Certain medications can increase the risk of bleeding in the gastrointestinal tract, even without causing structural damage.
Aspirin, non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen, and anticoagulants (blood thinners) can irritate the lining of the stomach and intestines, making bleeding more likely. Long-term use of these medications should be discussed with a healthcare provider.
Diet and lifestyle choices also play a role. Constipation from low fiber intake, excessive alcohol consumption, or heavy lifting can all contribute to minor rectal bleeding. These issues may not show up on a colonoscopy but can be addressed through changes in diet, hydration, and activity levels.
Functional and Microscopic Causes
Sometimes, bleeding results from conditions that are not visible during a standard colonoscopy.
Microscopic colitis is an inflammatory condition that affects the colon on a cellular level. It’s not visible to the naked eye but can be diagnosed through biopsies taken during the procedure. Though it more commonly causes watery diarrhea, in rare cases it may also lead to bleeding.
In rare instances, vascular malformations like angiodysplasia, abnormal, fragile blood vessels in the colon, might be missed if they’re small or not actively bleeding during the colonoscopy. These may require repeat imaging or specialized scans to detect.
Next Steps: When to Investigate Further
If bleeding continues or worsens, it’s important to follow up. Persistent or unexplained bleeding may call for additional tests such as:
- Repeat colonoscopy, especially if initial prep was suboptimal
- Upper endoscopy, to evaluate the esophagus, stomach, and duodenum
- Capsule endoscopy, where a small camera is swallowed to capture images of the small intestine
- CT angiography or nuclear medicine scans, which can detect active bleeding not visible by endoscopy
Your doctor will assess the pattern, frequency, and volume of bleeding to determine the urgency and direction of further testing.
Monitoring and Managing Symptoms
In many cases, when the cause of the bleeding is minor, like hemorrhoids or fissures, treatment is simple. Increasing fiber intake, staying well-hydrated, and using topical treatments can help resolve the issue over time.
Still, it’s important to track symptoms. Note the color of the blood, frequency of bleeding, any associated pain, changes in bowel habits, and whether it appears on or in the stool. These details can help your doctor narrow down the possible causes.
Conclusion
Finding blood in stools is never something to ignore, but a normal colonoscopy is often a strong indicator that there’s no serious underlying disease in the colon. However, it doesn’t always mean the investigation should stop there.
From minor anorectal issues to upper GI problems or microscopic conditions, there are several explanations that may not show up in a standard colonoscopy. The key is to stay proactive, work closely with your doctor, monitor your symptoms, and be open to further testing if needed.
With the right follow-up care and attention to possible causes, most cases of unexplained bleeding can be resolved or managed effectively.